*Content warning. This feature contains descriptions of pregnancy loss, hysterectomy and surgery
“We didn’t have children, I’d had an ectopic pregnancy in August 2015. I had emergency surgery. My heart stopped on the operating table. We lost the baby, and five months later I was diagnosed,” blogger and PhD researcher Fi Munro tells me. We are communicating via WhatsApp voice notes as she’s currently on the second of six rounds of chemotherapy. Her voice is positive and upbeat, despite me asking her to recount what happened when she was diagnosed with late stage ovarian cancer on January 18, 2016.
Symptoms: know your body
“I was really tired and I had a lot of abdominal bloating and pain,” Fi continues, listing the symptoms she had been experiencing. “I was going back and forward to my GP, because I knew there was something wrong. I even said it was ovarian cancer. I was told it was unlikely because I was only 30. They suggested it was a psychological response to the ectopic pregnancy, but I kept going back and demanded a scan.”
“Over 1,000 women under 50 are diagnosed every year, so it should never be ruled out just on the basis of your age,” affirms Catherine Murray, head of communications at the charity Target Ovarian Cancer, which has just launched a campaign, ‘It’s time to TAKE OVAR’, to help people recognise the symptoms. Unlike cervical cancer, which is picked up on a smear test, there is currently no screening for ovarian cancer; it’s a common misconception that the smear test will detect all gynaecological cancers.

There are four main symptoms of ovarian cancer:
- Persistent bloating
- Feeling full quickly/loss of appetite
- Stomach pain
- Needing to wee more often
“Swollen is a helpful word, as we often talk about bloating in relation to women’s bodies, especially during periods,” says Catherine, explaining why these symptoms get ignored or brushed aside. “It could start off small, so notice differences in your own body.”
Some other less well-known symptoms include back pain, pain during sex and a drop in energy levels. “But they are also the symptoms of lots of other illnesses and problems, especially for women,” Catherine continues. “It’s important to remember that when it’s ovarian cancer, these symptoms will be new for you, and they’re going to be persistent.”
It’s important to remember that when it’s ovarian cancer, these symptoms will be new for you, and they’re going to be persistent
“My periods started getting heavier around three or four months before I went to the doctor,” my friend Natalie Gee tells me. “I didn’t really think anything of it to start with. But I thought I should go and get it checked because it was different for me and my body.”
“I remember the appointment well. She asked me lots of questions: if I was in pain, if I could describe any other symptoms, how I was feeling…I was very tired at the time. But I’d just moved house and we were in the middle of renovating the whole place! Plus lots of women feel unwell when they’re on their period. I was also bloated but I put it down to my period. But it was worse than normal and different for me, so the GP must have picked up on it.”
“I actually thought I was gaining weight because my abdomen was growing bigger,” Fi tells me in another light-hearted voice note. “But I was eating less and becoming full quicker. This was due to a build-up of fluid, which they thought was an infection at first. They drained almost five kilos of fluid and underneath I was skeletal.”
A date with diagnosis
A month after her appointment, Natalie got a letter inviting her for a transvaginal ultrasound, where a small probe is inserted into your vagina to see your reproductive organs. She went along on her own, as she didn’t think there was anything to worry about – she didn’t even consider that it was cancer at this point. “I knew straight away that something was wrong. The person doing the scan looked shocked. As soon as I saw her face drop, I was worried,” Natalie tells me. “She could see two cysts on my ovaries, but I could tell by her face that there was more to it than that.”
When Natalie left, feeling unsure, she called on “Dr Google”. “Ovarian cancer came up online when I searched, but it seemed like an older woman’s disease, and I knew cysts didn’t necessarily mean cancer,” she says. But shortly after her scan, she was called back to have a CA125 blood test, which tests the levels of the protein in your blood. The normal range for CA125 is between 1 and 35. “My reading was more than 3,000. I didn’t know what that meant but I knew it was bad.”
For Fi, a phone call came an hour after the fluid was drained. “I will never forget it. I was sitting in the car in Asda car park about to go in and do the shopping. It was the first time the consultant had asked me to come in with someone else. I knew then that it was bad news, and I had been saying for weeks that it was cancer. I cried all the way home.”
“I remember sitting on the blue sofas in the gynaecology ward at the hospital opposite the consultant,” Fi continues matter of factly. “He told me that the fluid contained ovarian cancer cells. They said due to my symptoms that it was likely to be incurable and inoperable. I turned to my husband and said at least we can get a dog now I’m signed off work.”
Treatment options and dealing with the aftermath
Treatment differs for everyone, depending on what stage they are diagnosed at. Natalie found that as soon as she was diagnosed, things accelerated at a rapid pace and those few weeks of her life are “a bit of a blur.” She had to have a total abdominal hysterectomy. “That means everything: cervix, uterus, fallopian tubes, ovaries, and the two tumours,” says Natalie, who doesn’t have any children. “Tumours on both ovaries meant nothing could be preserved. And doing anything to save the eggs might risk a spread of cancer. I didn’t think it was a massive thing at the time. It seemed so secondary to everything else. There was no question that there was any other way to go about things.” Natalie did not need chemotherapy, and was told that everything was removed during surgery, the cancer was discovered when it was at stage 1 and had not spread.
Fi’s experience was different. “I’ve had chemo, alongside Avastin (a cancer treatment drug) as well as a major operation to remove my womb, cervix, fallopian tubes, ovaries, spleen, appendix, omentum, part of my bowel – I now have a colostomy bag – part of my diaphragm, part of my pancreas, part of my liver and multiple abdominal lymph nodes.” Fi talks about living with terminal cancer in her book How Long Have I Got? “My treatment now isn’t to cure me, my cancer is still terminal and untreatable. I’m talking about quality of life now rather than quantity.”
After my operation, I don’t think anyone even mentioned surgical menopause. I was told to “go off and enjoy my life”
“After my operation, I don’t think anyone even mentioned surgical menopause. I was told to ‘go off and enjoy my life’,” Natalie says, but she was about to deal with the huge and life-changing side effects of her major surgery, not to mention the months of agonising recovery. “I went from feeling one way to the complete opposite overnight. Menopause can be debilitating,” Natalie tells me. She’d received leaflets detailing every part of the process and support for everything else, apart from menopause. “The tiredness is most shocking. Some mornings, I felt so exhausted I didn’t want to get out of bed. In meetings, my brain felt so foggy I couldn’t contribute. I had always been confident at work, so I didn’t like how it affected me. It made me feel old, middle-aged.”
Natalie found support from other women online instead, including model Elly Mayday. However following other women diagnosed at different stages meant watching some of them die. “Elly had the same scar as me, which goes all the way down from my chest to my groin, and was the first younger woman I followed on Instagram who had ovarian cancer. I think she was diagnosed in 2013 at stage 3. She died last year.”
Stigma, stereotypes and redefining life
Natalie and Fi are far from the “cancer stereotypes” that we all know. They aren’t “battling” cancer, they aren’t sword-wielding warriors who are “fighting” a disease. They are dealing with their own realities. Yes, they are brave and strong and inspirational, but they had no other choice.
“Because I look ‘well’ people often don’t realise how ill I am,” says Fi when I ask her about misconceptions she’s faced. “Cancer doesn’t make you look ill, but the treatment can. It’s insulting when people say, ‘oh but you look so well.’ Because I might be in agony or maybe I have been up all night vomiting. I am a 34-year-old woman who looks healthy, so the judgment is upsetting.” Fi often documents the truth on her no-bullshit Instagram account, @fkmunro.
And be careful of the language you use when you talk to people who have cancer. Although Natalie’s was discovered at an early stage, she doesn’t feel “lucky”. “People say I am lucky all the time,” Natalie says. “And I am grateful. I am glad I didn’t have to have chemo, but I have still been through so much, I don’t think lucky is the right word.” But she doesn’t want sympathy. “I’ve got a nice life, an amazing husband, a good job, a beautiful house, loyal friends.” And because she is a married woman in her 30s, she often gets asked that dreaded question, when are you going to have kids? “If I turn round to someone and say: ‘well actually, I’ve had cancer and had to have a hysterectomy.’ That person is going to feel awful. Before I might have avoided that, but now I’m just honest.”
For Fi, cancer has given her a new outlook on life – and death. “We’re all terminal, we could all die at any point,” Fi explains. “We live our lives thinking we will live forever, but now I have this insight. I live my life knowing that it could end at any point. My motto is to live life like you’re dying.”
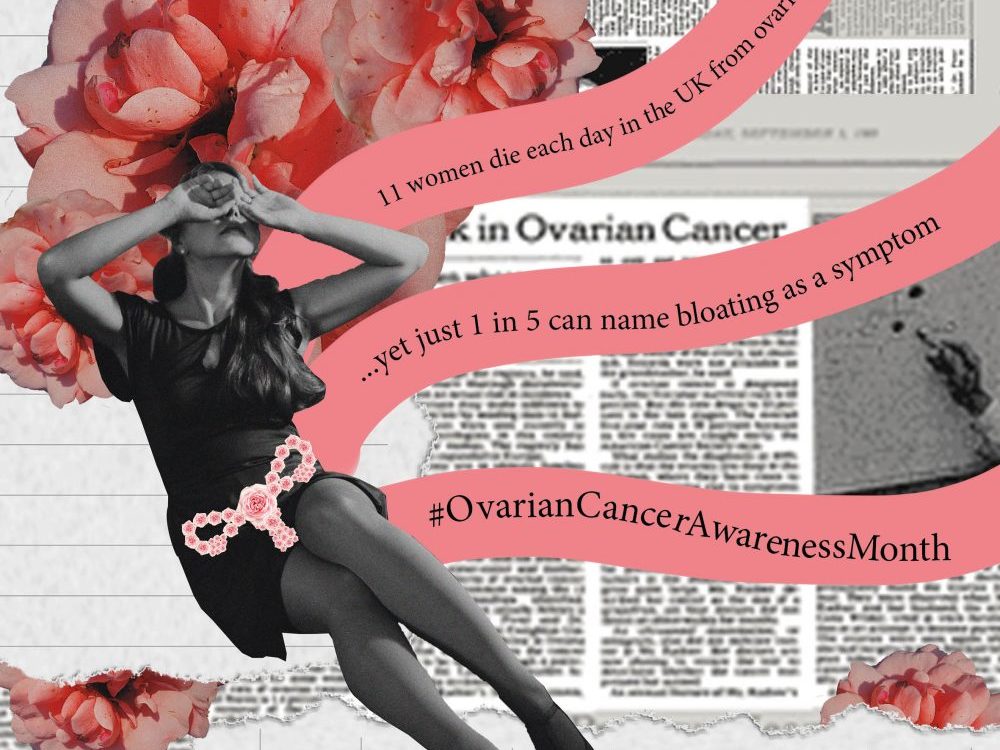
11 women die each day in the UK from ovarian cancer, yet just 1 in 5 can name bloating as a symptom
We should never, ever refer to ovarian cancer as a “silent killer” as it has been dubiously nicknamed, because it is a dangerous narrative and there ARE signs. And when a woman is diagnosed at the earliest stage, her chance of surviving ovarian cancer for five years or more doubles. So I asked Catherine from Target Ovarian Cancer what the main message is for young women: “Know the symptoms, tell your friends, tell your family, be aware of changes in your own body and stand up for your own health,” she asserts.
“It’s a misconception that young people don’t get cancer,” Fi passionately agrees. “I want to break down the embarrassment and stigma people have about their bodies so that people actually go to the doctors and speak to them. Not just that, but they speak up when the doctor says they are too young.”
“I recently chatted to my friend about my symptoms before I was diagnosed and she said she had noticed me being really tired as I’d kept cancelling plans, which isn’t like me,” says Natalie. So we must look out for each other, too. If your friend doesn’t seem like her usual joyous self, ask her how she is feeling, it might just make her stop and think. And most importantly of all: We must know our bodies, we must talk to each other, we must be unashamed.
Ovarian Cancer Awareness Month runs throughout March. There are unacceptable delays in ovarian cancer diagnosis which means one in five women diagnosed with ovarian cancer are already too ill for treatment. Target Ovarian Cancer is calling on UK governments to commit to action. Join the call to demand earlier diagnosis for ALL women. If you are worried about anything raised in this feature, contact Target Ovarian Cancer’s support line